Brain Injury Center
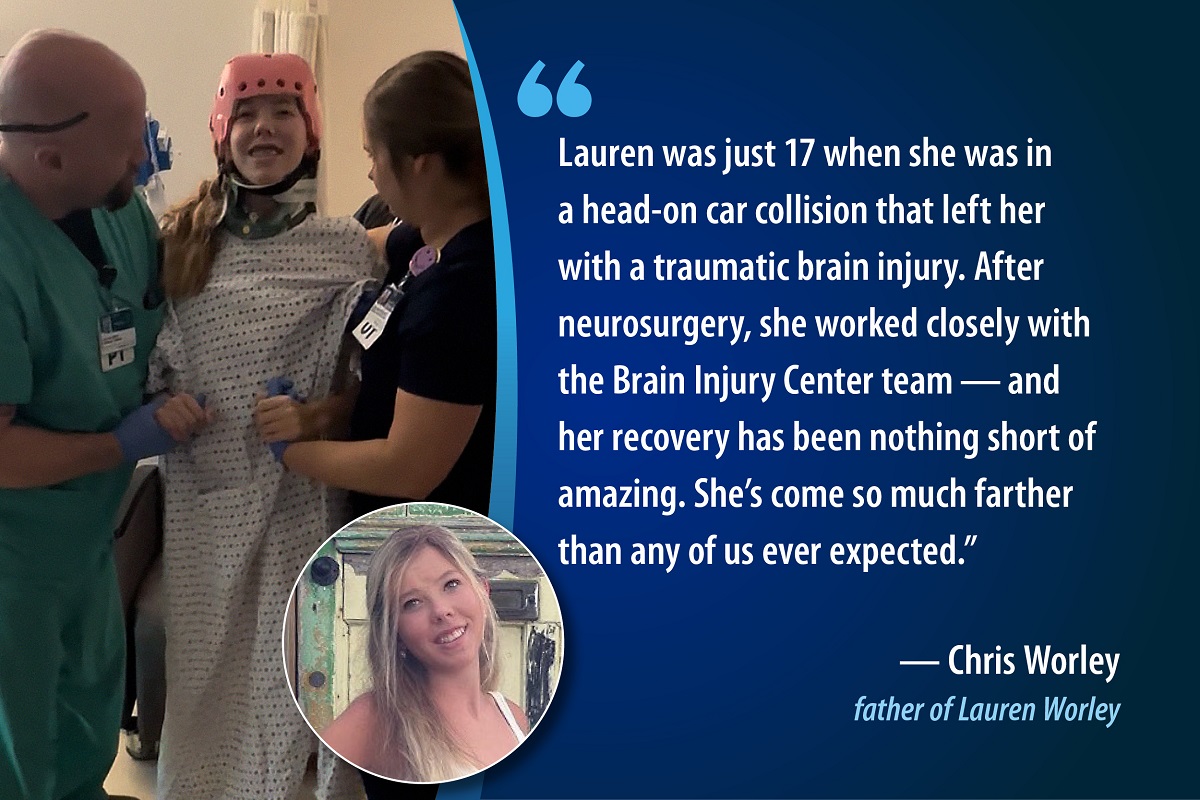
At Carilion, we are proud to offer a multidisciplinary team of experts to treat traumatic brain injuries (TBIs) focused on one shared goal: helping patients improve their quality of life.
Our Difference
TBIs affect every age group and vary in level of severity. Carilion's treatment goes beyond an initial diagnosis or treatment. We follow the National Academy of Medicine guidelines for treating the whole patient and their ongoing needs.
This includes:
- Follow-up care
- Multidisciplinary rehabilitation following an injury
- Continued evaluations to determine risks and decline in health and function
- Care to treat other health concerns such as mental health disorders
- Assistance with social needs, such as return to work.
Find out more by calling 540-224-5170.
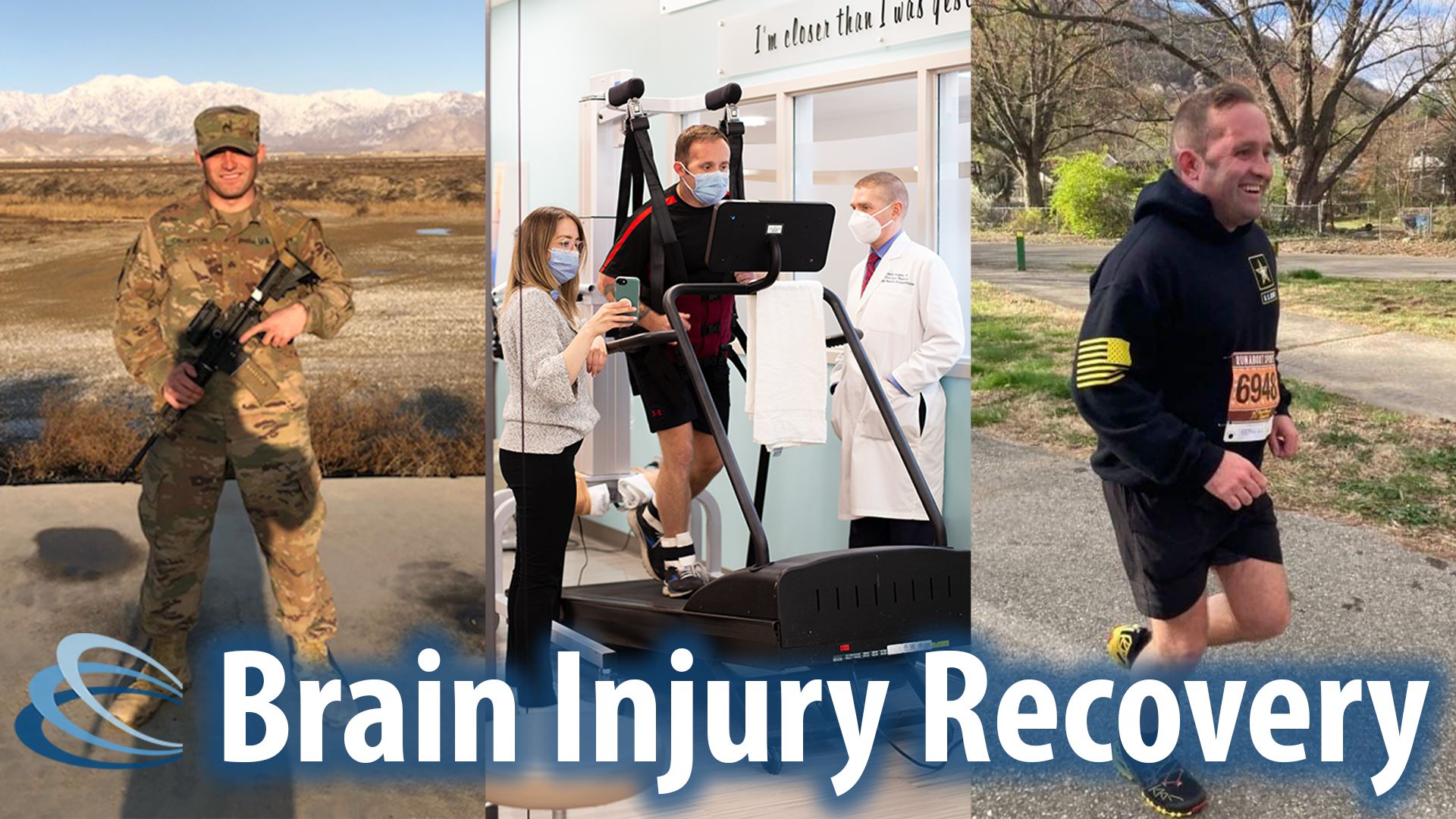
Traumatic Brain Injuries
Traumatic brain injuries (TBIs) can be the result of falls, sports injuries, car accidents or military combat. Each year, it is estimated that over 2 million people experience a TBI in the United States. For the number of TBIs recorded each year, the associated lifetime financial costs, including health care, lost income and reduced quality of life have been projected to be as high as $750 billion. Many people with TBI also find themselves without follow-up care, resulting in additional challenges that could have been avoided with a quality treatment program.
Services We Offer
Our brain injury center offers a variety of diagnostic tests and treatments to help improve your life.
- High intensity gait training
- A rigorous form of physical therapy designed to improve walking ability and speed in patients with gait impairments
- Glucagon stimulation test
- A diagnostic test used to assess the function of the pituitary gland by measuring its ability to secrete growth hormone in response to glucagon
- Impact testing
- Botox for migraines
- Botox for spasticity
- Occipital nerve blocks
- Trigger point injection
- Vagal nerve stimulators for seizures and depression
- Devices implanted under the skin that send electrical impulses to the vagus nerve to help control seizures and improve mood in patients with resistant depression
- Trigeminal nerve stimulators
- Neurorehabilitation
Meet Our Team
Our interdisciplinary team integrates multiple specialties through collaboration. We ensure that you receive the best care following a TBI and we understand the uncertainty and fear that can accompany concussions and other brain injuries. We know that you have questions about your symptoms and prognosis, and our accomplished team of highly trained specialists is here to provide you with the answers you need.
Our team has experience to diagnose and treat concussions and post-concussion syndrome, comprehensive brain injury management and muscle spasticity.

Justin L. Weppner, D.O.
Brain Injury Medicine
Physical Medicine and Rehabilitation
Emily Hillaker, D.O.
Brain Injury Medicine
Pediatric Physical Medicine and Rehabilitation
Mounica Thootkur, M.D.
Brain Injury Medicine
Psychiatry
Physical Therapy
Rehabilitation After a Brain Injury

Meet Stefanie Watts
Physical Therapist Stefanie Watts is dedicated to helping patients regain independence and improve their quality of life at our Brain Injury Center. As a seasoned specialist, she completed a Doctor of Physical Therapy degree from Medical University of South Carolina. Specializing in conditions such as stroke, brain injury, and vestibular disorders, Stefanie utilizes evidence-based physical therapy techniques to restore function and mobility. Her compassionate care focuses on empowering patients to overcome challenges and successfully return to their daily activities.
Why choose physical therapy at Carilion’s Brain Injury Center?
- We provide exceptional, passionate, neurologically specific care for our patients.
- Our therapists are well-versed in the most current best-practice for people with brain injuries.
- Our innovative model for physical therapy is heavily based in inter-disciplinary collaboration focused on a patient’s holistic wellness.
What types of brain injuries can benefit from physical therapy?
- Traumatic Brain Injuries (including concussions)
- Anoxic or Hypoxic Brain Injuries
- Strokes
- Brain Tumors
- People Recovering from Sundry Brain Surgeries
- Brain Cancer Survivors
- Adults living with Cerebral Palsy
Oversight by a skilled Physical Therapist is crucial in managing and recovering from all these conditions
How does physical therapy help after a brain injury?
Physical Therapists are movement experts and provide vital functions within the greater inter-disciplinary healthcare team including but not limited to:
- Patient education
- “dosed” exercise
- Manual/manipulative treatment
- Functional movement
- Identification and correction of movement patterns
- Gait (walking) rehabilitation at all levels
- Management and perspective on all aspects of a patient’s ability to move
- This is regularly communicated to the greater interdisciplinary healthcare team to inform the rest of the team’s decision making for the patient’s holistic recovery
These interventions can help to improve such symptoms as:
- Dizziness
- Headaches
- Problems concentrating
- Fatigue
- Whiplash & neck pain
- Joint & muscle stiffness
- Muscle weakness & contractures
- Problems with coordination and balance
- Inability to walk
How does physical therapy help with a brain injury?
Specific and individually “dosed” movement is a gold-standard, robustly researched panacea for many issues. Through a combination of neuro-cognitive, neuro-chemical, hormonal, muscular and neurologic mechanisms, movement can vastly improve the ability to live a meaningful and fulfilling life. Treatments focus on the above-mentioned interventions, and a Physical Therapists’ involvement and oversight ensures that a patient’s ability to independently move and interact with their environment in a meaningful way will always be a priority for the greater healthcare team.
Speech Therapy
Rehabilitation After a Brain Injury

Meet Kimberly Smiley
Originally from a small town in Western Pennsylvania, Kimberly has always had a passion for helping others. Throughout her junior/senior year of high school, she dedicated her free class time to shadow the Speech Pathologist within her hometown school district. Kimberly attended Clarion University of Pennsylvania where she earned her Undergraduate and Master’s Degree in Communication Sciences and Disorders. Upon graduating in 2006, she practiced Speech Language Pathology in Pennsylvania and throughout the Carolinas. Clinical settings have included skilled nursing facilities, assisted living facilities, and a Trauma 1 hospital system.
Kimberly is certified as a Brain Injury Specialist with clinical competence in both evaluation and treatment of Cognitive-Linguistic Impairments and Dysphagia. She strives to provide compassionate person-centered care to those living with Neurological Disorders to include Brain Injury, Stroke, and Dementia.
Outside of work, Kimberly enjoys music, movies, attending sporting events/concerts, crafts, traveling, and most importantly, spending time with her family, husband (Phil) and her dog (Gus).
Why Choose Speech Therapy at Carilion Clinic’s Brain Injury Center?
Our Speech Language Pathologist embraces an interdisciplinary team approach while implementing up to date clinical practice guidelines for the evaluation and treatment of cognitive-communicative, language, and swallowing disorders related to neurological impairments. As a Certified Brain Injury Specialist (CBIS), our clinician strives to provide the highest level of education, compassion, and treatment approaches to our patients and their families to support independence and reintegration within the community.
Speech Therapy Services and Outpatient Brain Injury Rehabilitation:
As part of the continuum of care, Outpatient Speech Language Pathologists serving Carilion Clinic’s Brain Injury Center are healthcare professionals trained to assess and provide treatment/strategies for the following disorders as they relate to brain injury/neurological involvement:
- Receptive and Expressive Language Disorders -Impairments in understanding auditory/written/visual information and expressing wants/needs/ideas.
- Cognitive Disorders-Impairments in concentration, attention, memory, reasoning, and thought organization.
- Voice Disorders/Dysarthria-Impairments in production and/or articulation of speech sounds.
- Dysphagia- Impairments in swallowing function.
Occupational Therapy
Rehabilitation After a Brain Injury

Meet Crystal Gibson
Crystal Gibson is an occupational therapist who specializing in neurological diagnoses. She is a licensed and registered occupational therapist in the state of Virginia and a member of the American Occupational Therapy Association (AOTA). She is actively involved with research on stroke recovery with special interest in the use of transcranial magnetic stimulation as a diagnostic tool and interdisciplinary use of outcome measures. Crystal received her bachelor's of science degree from East Carolina University in therapeutic recreation and her master's degree in science from Jefferson College of Health Sciences in occupational therapy.
She spent the initial part of her career working in the greater Roanoke Valley, with the brain injury population, as a case manager and life skills trainer before joining Carilion in 2012 as an occupational therapist. For the past 11 years, Crystal has worked in physical rehabilitation on an inpatient unit, where she gained experience working with a multitude of diagnoses. Her primary interest in motor and neurological dysfunction includes; stroke, brain injury, and spinal cord injury. Crystal is excited to be part of the Brain Injury Center’s outpatient setting to provide evidence-based therapeutic interventions with a focus on vision rehabilitation, to improve their well being and overall independence. Outside of work, Crystal enjoys spending time with her husband and three children camping, taking walks, bowling, and traveling to the best beaches.
Why Choose Occupational Therapy at Carilion Clinic’s Brain Injury Center?
The primary goal of occupational therapy at the Brain Injury Center is to improve one’s independence and participation in activities of everyday life. Our occupational therapy department focuses on patient’s individual goals to aid in regaining independence in self care, use of adaptive equipment, compensatory strategies, ocular motor function, and functional mobility to enhance overall well-being and quality of life.
Our occupational therapist embraces a holistic and interdisciplinary team approach. She follows clinical practice guidelines in technology, and evidence-based practice for the evaluation and treatment of neurological deficits. Deficits commonly treated include oculomotor retraining, motor impairments, cognitive and perceptual impairments, and support of neuromusculoskeletal integrity related to neurological impairments.
As an occupational therapist, our clinician strives to provide compassionate care to help patients regain their independence and reintegration into the community.
Occupational Therapy Services and Outpatient Brain Injury Rehabilitation:
As part of the continuum of care, outpatient occupational therapist serving Carilion Clinic’s Brain Injury Center are healthcare professionals trained to assess and provide treatment/strategies for the following disorders as they relate to brain injury/neurological involvement:
- Motor impairments: hemiplegia, hemiparesis, postural control, contractures, coordination, functional reach.
- Visual deficits: visual field deficits, double vision, light sensitivity, visual inattention (neglect), ocular motor deficits.
- Cognitive and perceptual impairments
- Sensory impairments
- Activities of Daily living: dressing, bathing, toileting, grooming, self-feeding.
- Independent Activities of Daily Living: Cooking, cleaning, household management, vocational skills.
Stroke Recovery
After a stroke, more than half of survivors still have trouble moving their arms and hands. We're now offering patients a new option, even if therapy didn't help previously. A small, implanted device helps stroke survivors regain hand and arm function when used in combination with occupational therapy. Learn more about our Enhanced Stroke Recovery Program.
Growth Hormone Issues
A traumatic brain injury (TBI) can impact more than just your brain—it may also affect your hormones. The pituitary gland, located just beneath the brain, can be damaged during a TBI, leading to hormone imbalances such as growth hormone deficiency. Learn more about this important connection.
Neurorehabilitation
Neurorehabilitation at Carilion Clinic’s Brain Injury Center
Neurorehabilitation, or neurorehab, is a specialized therapeutic approach aimed at improving the lives of individuals with acquired brain injuries such as stroke and traumatic brain injury. This comprehensive care combines medical, physical, and psychological therapies to enhance patients' quality of life and independence.
Key Components:
· Medical Management: Continuous monitoring and intervention to address medical needs.
· Physical Therapy: Exercises to improve mobility, strength, and balance.
· Occupational Therapy: Techniques to enhance daily living activities and motor skills.
· Speech and Language Therapy: Support for communication difficulties and cognitive impairments.
· Psychological Support: Counseling to cope with emotional and psychological challenges.
· Technological Aids: Advanced tools like virtual reality.
· Exceptional Care: Neurologically specific care using current best practices.
· Interdisciplinary Collaboration: Holistic wellness through teamwork.
· Conditions Treated: Traumatic brain injuries, anoxic/hypoxic injuries, strokes, brain tumors, post-surgery recovery, brain cancer survivors.
Benefits:
· Improved Functional Outcomes: Greater independence in daily activities.
· Enhanced Quality of Life: Better symptom management and well-being.
· Personalized Care: Customized treatment plans for each patient.
· Interdisciplinary Approach: Comprehensive care from a team of specialists.
Therapy Services in the Brain Injury Center :
· Physical Therapy: Movement experts providing patient education, dosed exercise, manual treatment, functional movement, and gait rehabilitation. Helps with dizziness, headaches, concentration issues, fatigue, neck pain, joint stiffness, muscle weakness, coordination, balance, and walking.
· Speech Therapy: Interdisciplinary team and certified brain injury specialists offering compassionate care. Treats receptive/expressive language disorders, cognitive disorders, voice disorders, and dysphagia.
· Occupational Therapy: Focus on improving independence in daily activities through addressing motor, visual, cognitive, perceptual, and sensory impairments. Assists with dressing, bathing, grooming, self-feeding, and household management.
Research
Scholarly and Professional Publications
Book
Wagner A.K.; Weppner J., (Apr 08, 2024). Acute care neuroconsultation and neurorehabilitation management. Acute Care Neuroconsultation and Neurorehabilitation Management 1 - 326 doi: 10.1007/978-3-031-42830-2. Published
Journal Article
Shick T.; Perkins C.; Paul A.; Martinez M.; Joyce J.; Beach K.; Swahlan J.; Weppner J., (Jan 24, 2025). Randomized Controlled Trial: Preliminary Investigation of the Impact of High-Intensity Treadmill Gait Training on Recovery among Persons with Traumatic Brain Injury. Neurotrauma Reports 6 82 - 92 doi: 10.1089/neur.2024.0169. Published
Awan N.; Weppner J.; Kumar R.; Juengst S.; Dams-O'Connor K.; Sevigny M.; Zafonte R.; Walker W.; Szaflarski J.; Wagner A., Impact of Post-Traumatic Epilepsy on Mental Health and Multidimensional Outcome and Quality of Life: An NIDILRR TBIMS Study. Journal of Neurotrauma doi: 10.1089/neu.2024.0117. Published online
Ladner L.; Shick T.; Adhikari S.; Marvin E.; Weppner J.; Kablinger A., (Dec 02, 2024). Association between impulsivity and suicide in traumatic brain injury patients. Journal of Neurotrauma 41 2580 - 2589 doi: 10.1089/neu.2024.0167. Published
Weppner J.; Yim I.; Raucheisen J.; Martinez M., (Oct 02, 2024). A Survey to Determine Health Utility States After a Traumatic Brain Injury (TBI): Influence of a History of TBI on Disability Perceptions. Cureus 16 e70707 - e70707 doi: 10.7759/cureus.70707. Published
Weppner J.; Senol S.; Larick R.; Jackson S., Diagnostic Accuracy of the Yale Swallow Protocol in Moderate-to-Severe Traumatic Brain Injury: A Prospective Blinded Videofluoroscopic Investigation. Journal of Head Trauma Rehabilitation 39 E393 - E398 doi: 10.1097/HTR.0000000000000929. Published online
Weppner J.; Zhang J.; Fan E.; Awan N.; Linsenmeyer M.; Conley Y.; Grafman J.; Wagner A., (May 31, 2024). Characterizing Genetic Risk Factors for Post Traumatic Epilepsy Following Combat Brain Injury. (Abstract) The Journal of Head Trauma Rehabilitation 9 - 10 doi: 10.1097/HTR.0000000000000963. Published
Weppner J.; Conti A.; Locklear T.; Mayer R., (May 17, 2024). Traditional Lecture Versus Procedural Video Randomized Trial: Comparative Analysis of Instructional Methods for Teaching Baclofen Pump Management. American Journal of Physical Medicine & Rehabilitation 103 510 - 517 doi: 10.1097/PHM.0000000000002397. Published
Mishra V.; Bath J.; Harvey E.; Martinez M.; Gorton L.; Collier B.; Weppner J., (May 01, 2024). Factors Impacting Mortality and Withdrawal of Life Sustaining Therapy in Severe Traumatic Brain Injury. (Abstract) American Journal of Physical Medicine & Rehabilitation S268 - S269 doi: 10.1097/PHM.0000000000002459. Published
Shick T.; Perkins C.; Paul A.; Martinez M.; Joyce J.; Beach K.; Swahlan J.; Bonner R.; Homan E.; Lynn R.; Wadding J.; Weppner J., (May 01, 2024). Preliminary Investigation: Evaluating the Impact of High-Intensity Treadmill Gait Training on Locomotion Recovery in Traumatic Brain Injury. (Abstract) American Journal of Physical Medicine & Rehabilitation 103 S80 - S80 doi: 10.1097/PHM.0000000000002459. Published
Bath J.; Barylak M.; Kedda E.; Harvey E.; Locklear T.; Martinez M.; Collier B.; Weppner J., (Mar 24, 2024). Timing of Withdrawal of Life-Sustaining Therapy in Traumatic Brain Injury: Exploring Indicators of Poor Prognosis in Adult and Geriatric Populations. Brain Injury 38 267 - 272 doi: 10.1080/02699052.2024.2309656. Published
Weppner J.; Gee A.; Mesina K., (Feb 21, 2024). Enhancing Safety in the Ischaemic and Haemorrhagic Stroke Population: Exploring the Efficacy of Self-releasing Chair Alarm Belts. BMJ Open Quality 13 1 - 6 doi: 10.1136/bmjoq-2023-002569. Published
Weppner J.; Hillaker E.; Boomgaardt J.; Tan S.; Holum P.; Li F.; Tu J.; Sheppard M., (Oct 20, 2023). Actigraphic and Sleep Log Measures in Moderate-to-Severe Traumatic Brain Injury: Identifying Discrepancies in Total Sleep Time. PM&R 15 1266 - 1272 doi: 10.1002/pmrj.12934. Published
Weppner J.; Wray M., (Sep 29, 2023). A Survey to Determine Health Utility States After a Hypothetical Traumatic Brain Injury: The Influence of the Personal History of Severe Traumatic Brain Injury on Disability Perceptions. (Abstract) Brain Injury 37 36 - 36 doi: 10.1080/02699052.2023.2247822. Published
Weppner J.; Wray M., (Sep 29, 2023). A Survey of Physician Perceptions of Disability Outcomes After Hypothetical Traumatic Brain Injury. (Abstract) Brain Injury 37 41 - 42 doi: 10.1080/02699052.2023.2247822. Published
Bath J.; Harvey E.; Collier B.; Weppner J., (Sep 29, 2023). Mortality Associated with Withdrawal of Life-sustaining Therapy for Patients with Severe Traumatic Brain Injury: A Retrospective Single-center Study. (Abstract) Brain Injury 37 124 - 124 doi: 10.1080/02699052.2023.2247822. Published
Weppner J.; Khan A.; Raucheisen J., (Aug 26, 2023). Pheochromocytoma-Induced Hypertension After Traumatic Brain Injury. Cureus 15 1 - 3 doi: 10.7759/cureus.44161. Published
Weppner J.; Jain A.; Kim H.S., (Jul 13, 2023). Infectious Encephalopathies and Leukoencephalopathies: An Updated Review. PM&R Knowledge NOW Published online
Weppner J., (Apr 01, 2023). Feasibility, Reliability and Validity of A Baclofen Pump Rubric For Evaluating Baclofen Pump Refilling and Programming. (Abstract) American Journal of Physical Medicine & Rehabilitation 102 a69 - a69 doi: 10.1097/PHM.0000000000002184. Published
Weppner J.; Barge K.; Gibson C.; Kroese L.; Woolson E.; Beach K., (Apr 01, 2023). The Use of Self-Releasing Chair Alarm Belts in the Ischemic and Hemorrhagic Stroke Population. (Abstract) American Journal of Physical Medicine & Rehabilitation 102 a84 - a84 doi: 10.1097/PHM.0000000000002184. Published
Hillaker E.; Lau J.; Boomgaardt J.; Weppner J., (Jan 01, 2023). Metronidazole-Induced Neurotoxicity: A Clinical Vignette. Medicine: Case Reports and Study Protocols 4 e0268 - e0268 doi: 10.1097/MD9.0000000000000268. Published
Tate K.; Pellegrino V.; Goodwin C.; Weppner J.; Marks M.; McDaniel B., (Jan 01, 2023). 514: Evaluation Of Amantadine On Cognitive Outcomes In Traumatic Brain Injury Patients. (Abstract) Critical Care Medicine 51(1) 244 - 244 doi: 10.1097/01.ccm.0000907784.42226.2a. Published
Weppner J.; Jackson S.; Marks M., (Dec 01, 2022). Validation of the Yale Swallow Protocol in Traumatic Brain Injury: A Prospective Videofluoroscopic Study. (Abstract) Journal of Head Trauma Rehabilitation 37(6) E514 - E514 doi: 10.1097/HTR.0000000000000845. Published
Weppner J., (Jul 01, 2022). Construct Validity of the Resident Observation and Competency Assessment. (Abstract) American Journal of Physical Medicine and Rehabilitation 101 a1 - a1 doi: 10.1097/PHM.0000000000002036. Published
Anzivino A.; Weppner J., (Jul 01, 2022). Utilizing the Telephone Effect to Assess a Patient With Akinetic Mutism Following Traumatic Brain Injury. (Abstract) American Journal of Physical Medicine & Rehabilitation 101 a156 - a156 doi: 10.1097/PHM.0000000000002036. Published
Weppner J.; Hillaker E.; Boomgaardt J., (Nov 14, 2021). Case Report: Regaining Function After Metronidazole-induced Cerebellar Toxicity. (Abstract) PM&R 13 doi: 10.1002/pmrj.12735. Published
Weppner J.L.; Linsenmeyer M.A.; Wagner A.K., (Nov 01, 2021). Acute Care Brain Injury Medicine Continuity Consultation Service Associations with Healthcare Utilization and Rehabilitation Outcomes Among Individuals with Acquired Brain Injury. PM&R 1227 - 1236 doi: 10.1002/pmrj.12563. PMID: 33527710. Published
Bova M.; Tu J.; Chang A.; Weppner J., (Oct 13, 2021). Delayed Onset Neurologic Deterioration Following Traumatic Brain Injury. Medicine: Case Reports and Study Protocols 1 - 4 doi: 10.1097/MD9.0000000000000167. Published
Peacock F.; Kuehl D.; Diaz-Arrastia R.; Vanlandingham J.; Than M.; Canon C.; Singer A.; Mirshahi N.; Weppner J.; Gerwien R., TBI Presentations Associated with Persistent Symptoms. Journal of Neurotrauma Submitted
Professional Organization Presentations
Conference Paper or Presentation
International
Kuehl D.; Van Meter T.; Roscovsky K.; Diaz-arrastia R.; Weppner J.; Mirshah N., "Geriatric Acute TBI and Dementias Differ in Blood Biomarker Profiles: Results from the HeadSMART Geriatric Feasibility Study", International Neurotrauma Society Annual Meeting, Cambridge, England (Sep 04, 2024)
Weppner J., "Characterizing Genetic Risk Factors of Seizures Following Traumatic Brain Injury", International Conference for Post-Traumatic Epilepsy, Milan, Italy (May 17, 2024)
Van Meter T.; Mirshah N.; Sandsmark D.; Roscovsky K.; Diaz-Arrastia R.; Weppner J.; Kuehl D., "Biomarker Profiles Distinguish Geriatric Acute TBI from Dementias: Results from the HEADSMART Geriatric Feasibility Study", International Conference on Alzheimer’s and Parkinson’s Diseases, Lisbon, Portugal (Mar 05, 2024)
Weppner J., "A Survey to Determine Health Utility States After a Hypothetical Traumatic Brain Injury: The Influence of the Personal History of Severe Traumatic Brain Injury on Disability Perceptions", International Brain Injury Association, Dublin, Ireland (Apr 01, 2023)
Weppner J., "A Survey of Physicians' Perceptions of Disability Outcomes After Hypothetical Traumatic Brain Injury", International Brain Injury Association, Dublin, Ireland (Mar 31, 2023)
Weppner J.; Jackson S., "Validation of the Yale Swallow Protocol in Traumatic Brain Injury: A Prospective Videofluoroscopic Study", 2022 Joint Conference on Brain Injury, North American Brain Injury Society (NABIS) and International Paediatric Brain Injury Society (IPBIS), New York, NY (Sep 23, 2022)
National
Paul A.; Perkins C.; Shick T.; Joyce J.; Beach K.; Swahlan J.; Bonner R.; Homan E.; Lynn R.; Wadding J.; Weppner J., "Efficacy of High Intensity Gait Training in Traumatic Brain Injury: A Pilot Randomized Controlled Trial", 2025 American Physical Therapy Association Combined Sections Meeting, Houston, TX
Weppner J., "Diagnosis and Treatment of Sialorrhea and Oromandibular Dystonia in Adult and Pediatric Patients: Ultrasound Guided Injections", 2024 AAPM&R Annual Meeting, American Academy of Physical Medicine and Rehabilitation, San Diego, CA (Nov 08, 2024)
Weppner J., "Ultrasound-guided Injections for Salivary Glands and Oromandibular Dystonia", 2024 AAPM&R Annual Meeting, American Academy of Physical Medicine and Rehabilitation, San Diego, CA (Nov 07, 2024)
Weppner J., "Pacira Resident Experience", 2024 AAPM&R Annual Meeting, American Academy of Physical Medicine and Rehabilitation, San Deigo, CA (Nov 07, 2024)
Weppner J.; Conti A.; Locklear T.; Mayer R., "Traditional Lecture Versus Procedural Video Randomized Trial: Comparative Analysis of Instructional Methods for Teaching Baclofen Pump Management", 2024 AAP Annual Meeting, Orlando, FL (Feb 23, 2024)
Shick T.; Perkins C.; Paul A.; Martinez M.; Joyce J.; Beach K.; Swahlan J.; Bonner R.; Homan E.; Lynn R.; Wadding J.; Weppner J., "Preliminary Investigation: Evaluating the Impact of High-Intensity Treadmill Gait Training on Locomotion Recovery in Traumatic Brain Injury", 2024 AAP Annual Meeting, Orlando, FL (Feb 23, 2024)
Weppner J.; Ide W.; Raiser S., "Exploring the Potential Applications of Artificial Intelligence in Medical Education and Practice: A Critical Analysis for Academic Physiatry Educators", 2024 AAP Annual Meeting, Orlando, FL (Feb 22, 2024)
Weppner J., "Construct Validity of the Resident Observation and Competency Assessment", 2022 AAP Annual Meeting, Association of Academic Physiatrists, New Orleans, LA (May 27, 2022)
Weppner J.; Raiser S.; Ide W.; Herman D., "Beyond ‘‘Read More'': A Workshop to Improve Written Feedback to Learners Using an Evidence- based Framework", 2022 AAP Annual Meeting, Association of Academic Physiatrists, New Orleans, LA (May 26, 2022)
Regional
Jennifer B.; Mishra V.; Harvey E.; Martinez M.; Gorton L.; Collier B.; Weppner J., "Factors Impacting Mortality and Withdrawal of Life Sustaining Therapy in Severe Traumatic Brain Injury", The Carolinas Virginias Chapter of the Society of Critical Care Medicine, Myrtle Beach, SC (Jun 14, 2024)
Bath J.; Harvey E.; Collier B.; Weppner J., "Mortality Associated with Withdrawal of Life-Sustaining Therapy for Patients with Severe Traumatic Brain Injury: A Retrospective Single-Center Study", Carolinas/Virginias Chapter of the SCCM's 41st Annual Scientific Symposium, Carolinas/Virginias Chapter of the SCCM's, Raleigh, NC (Jun 08, 2023)
State
Weppner J., "Understanding the Human Toll of Military TBI: One Marine's Story", Making Headway, The Brain Injury Association of Virginia, Roanoke, Virginia (Oct 29, 2022)
Local
Shick T.; Perkins C.; Paul A.; Martinez M.; Joyce J.; Beach K.; Swahlan J.; Bonner R.; Homan E.; Lynn R.; Wadding J.; Weppner J., "Preliminary Investigation: Evaluating the Impact of High-Intensity Treadmill Gait Training and Locomotion Recovery in Traumatic Brain Injury", Carilion Clinic Research Day 2024, Roanoke, VA (Apr 09, 2024)
Mishra V.; Harvey E.; Martinez M.; Gorton L.; Collier B.; Weppner J., "Factors Impacting Mortality and Withdrawal of Life Sustaining Therapy in Severe Traumatic Brain Injury", Carilion Clinic Research Day 2024, Roanoke, VA (Apr 09, 2024)
Weppner J., "Physiatric Approach to Stroke Rehabilitation: Effectiveness and Efficiency of Early Rehabilitation", Carilion Clinic Stroke Symposium Virtual Conference, Carilion Clinic, Roanoke, VA (May 16, 2022)
Weppner J., "Weathering the Storm After Acquired Brain Injury: Paroxysmal Sympathetic Hyperactivity", 72nd Annual Spring Symposium, Carilion Clinic, Roanoke, Virginia (Mar 24, 2022)
Poster
International
Kuehl D.R.; Sandsmark D.; Roscovsky K.; Diaz-Arrastia R.; Weppner J.; Boyd S.; Leinmuelle J.; Barton M.; Mirshahi N.; Van Meter T., "Geriatric Acute TBI and Dementias Differ in Blood Biomarker Profiles: Results from the HeadSMART Geriatric Feasibility Study", Meeting of the International Neurotrauma Society, Cambridge, United Kingdom (Sep 02, 2024)
Weppner J.; Awan N.; Linsenmeyer M.; Conley Y.; Wagner A., "Characterizing Genetic Risk Factors of Seizures Following Traumatic Brain Injury", International Conference for Post-Traumatic Epilepsy, Milan, Italy (May 16, 2024)
Weppner J.; Awan N.; Kumar R.; Juengst, S.; Harrison-Felix C.; Dams-O’Connor K.; Zafonte R.; Walker W.; Szaflarski J.; Wagner A., "Impact of Post Traumatic Epilepsy on Mental Health and Multidimensional Outcome and Quality of Life: An NIDILRR TBI MS Study", International Conference for Post-Traumatic Epilepsy, Milan, Italy (May 16, 2024)
Bath J.; Harvey E.; Locklear T.; Collier B.; Martinez M.; Barylak M.; Weppner J., "Mortality Associated With Withdrawal of Life-Sustaining Therapy for Patients with Severe Traumatic Brain Injury: A Retrospective Single-Center Study", International Brain Injury Association, Dublin, Ireland (Mar 31, 2023)
National
Paul A.; Perkins C.; Homan E.; Wadding J.; Lynn R.; Bonner R.; Shick T.; Martinez M.; Joyce J.; Beach K.; Glass S.; Weppner J., "Efficacy of High-Intensity Gait Training in Traumatic Brain Injury: A Pilot Randomized Controlled Trial", 50th Annual APTA CSM, APTA CSM, Housten, TX (Feb 15, 2025)
Van Meter T.; Mirshahi N.; Boyd S.; Sandsmark D.; Rascovsky K.; Diaz-Arrastia R.; Weppner J.; Kuehl D., "Development of distinct acute TBI and chronic neurodegeneration signatures for precise diagnostics in the elderly: Results from the HeadSMART Geriatric Study.", (Abstract) NINDS-DTR SBIR Neuroscience Satellite Meeting, National Institute of Neurological Disorders and Stroke, Chicago, IL (Oct 07, 2024)
Weppner J.; Zhang J.; Fan E.; Awan N.; Linsenmeyer M.; Conley Y.; Grafman J.; Wagner A., "Characterizing Genetic Risk Factors for Posttraumatic Epilepsy Following Combat Brain Injury", NABIS Conference on Brain Injury, Las Vegas, NV (Mar 28, 2024)
Mishra V.; Bath J.; Harvey E.; Martinez M.; Gorton L.; Collier B.; Weppner J., "Factors Impacting Mortality and Withdrawal of Life Sustaining Therapy in Severe Traumatic Brain Injury", 2024 AAP Annual Meeting, Orlando, FL (Feb 23, 2024)
Jain A.; Kim H.S.; Weppner J.; Simpson L., "Basal Ganglia Hemorrhage in a Patient with Upshaw-Schulman Syndrome: A Case Report.", New Orleans, LA (Nov 16, 2023)
Weppner J., "Feasibility, reliability and validity of a baclofen pump rubric for evaluating baclofen pump refilling and programming", Association of Academic Physiatrists Annual Meeting, Association of Academic Physiatrists, Anaheim, CA (Feb 22, 2023)
Weppner J.; Barge K.; Crystal G.; Lori K.; Elizabeth W.; Katy B., "The Use of Self-releasing Chair Alarm Belts in the Ischemic and Hemorrhagic Stroke Population", Association of Academic Physiatrists Annual Meeting, Association of Academic Physiatrists, Anaheim, CA (Feb 22, 2023)
Tate K.; Pellegrino V.; Goodwin C.; Marks M.; Weppner J.; McDaniel B., "Evaluation of Amantadine on Cognitive Outcomes in Traumatic Brain Injury Patients", 2023 Critical Care Congress, San Francisco, California (Jan 21, 2023)
Anzivino A.; Weppner J., "Case Report: Utilizing the Telephone Effect to Assess a Patient with Akinetic Mutism Following Traumatic Brain Injury", 2022 AAP Annual Meeting, Association of Academic Physiatrists, New Orleans, LA (May 27, 2022)
Hillaker E.; Boomgaardt J.; Weppner J., "Case Report: Regaining Function After Metronidazole-induced Cerebellar Toxicity", 2021 AAPM&R Annual Meeting, American Academy of Physical Medicine and Rehabilitation, Online Due to COVID-19 (Nov 11, 2021)
Local
Weppner J.; Rosenthal K.; Bath J.; Martinex M.; Locklear T., "IGF-1 as a Biomarker for Symptom Severity in Adult Traumatic Brain Injury: Evidence from an Observational Study", VCOM Research Day, Blacksburg, VA (Feb 14, 2025)
Mishra V.; Rosenthal K.; Hillaker E.; Martinez M.; Bath J.; Ide W.; Stodgehill J.; Locklear T.; Weppner J., "IGF-1 as a Biomarker for Symptom Severity in Adolescents with Traumatic Brain Injury", VCOM Research Day, Blacksburg, VA (Feb 14, 2025)
Weppner J.; Conti A.; Locklear T.; Mayer R., "Traditional Lecture Versus Procedural Video Randomized Trial: Comparative Analysis of Instructional Methods for Teaching Baclofen Pump Management", 2023 TEACH Education Day, Roanoke, VA (Oct 30, 2023)
Weppner J., "Construct Validity of the Resident Observation and Competency Assessment", 2021 TEACH Education Day, Teaching Excellence Academy for Collaborative Healthcare, Roanoke, Virginia (Oct 28, 2021)
Brain Injury Support Group

Join us for a supportive and engaging Brain Injury Support Group led by Carilion’s Brain Injury Center care team and the Keeley Healing Arts Program.
Artist-in-Residence Catherine Backus, MT-BC, will use music to encourage emotional expression, reduce stress, and promote well-being. She’ll be joined by fellow Artist-in-Residence Arianne Thompson, SLP, BFA, who will incorporate fun, simple rhythmic movements. Whether you’re a traumatic brain injury or stroke survivor, caregiver or family member, come connect, share and heal with others on a similar journey through the power of music and community support.
Join us!
First Wednesday of each month
Noon - 1 p.m.
Carilion Clinic Institute for Orthopaedics and Neurosciences
2331 Franklin Road SW, Roanoke, VA 24014
Conference room 5, Level 2
For more information, contact Lisa Linger, Keeley Healing Arts Program manager, at lmlinger@carilionclinic.org. Class participation is free.
Awards

Top Honors for Commitment to Patient Care
Among all Carilion Clinic departments and programs, the Brain Injury Center earned the Commitment Award, recognizing our team as top performers in 2025. This distinction highlights our exceptional dedication to patient care and success in advancing meaningful outcomes for those we proudly serve.
Thank you for trusting us with your care! To schedule an appointment, call 540-224-5170.