The Next Wave
Together Carilion Clinic and Blue Ridge Cancer Care are helping to pioneer a new method for treating cancer. Theranostics uses molecular radiotherapy to target and treat tumors with precision.
Anita Haymaker had already been through a lot. Several years ago, although she felt generally healthy, “I was breaking out all over,” she says. So she saw her doctor, who ordered tests that led to her first cancer diagnosis: a neuroendocrine tumor in her pancreas.
Haymaker had surgery to remove the tumor, but two years later the cancer returned, this time in her liver. She had another operation and, when the cancer came back again, she had a hysterectomy. “After that, my doctors said they didn’t think I was a candidate for any more surgery,” says Haymaker, who lives with her husband, Kenny, on Smith Mountain Lake, southeast of Roanoke.
But doctors found more cancer in Haymaker’s pancreas and liver, and she began receiving chemotherapy at Blue Ridge Cancer Care. That’s when her doctor suggested she see David Buck, M.D., president of Blue Ridge Cancer Care and medical director of Radiation Oncology at Carilion Clinic’s Cancer Center.
Dr. Buck also serves as chair of Carilion’s oncology committee and head of radiation research for the U.S. Oncology Network, of which Blue Ridge Cancer Care is a part. He was recruiting patients for a trial of a radioactive compound called lutetium dotatate.
In Haymaker’s meeting with Dr. Buck, he explained that this new treatment was being tested in patients whose tumors were no longer responding to other therapies. If she chose to participate in the trial, she would receive multiple treatments, spaced about six weeks apart. Although the infusion of the radioactive compound itself would take only half an hour or so, she would also receive intravenous amino acids before and after to help protect her kidneys, so she should expect to be at the clinic for most of the day for each treatment.
“He told me they would bring the drug in a little metal box because it was nuclear,” she remembers. She found that a little disconcerting, like something out of a science fiction movie. But with the effectiveness of other treatments fading fast, she felt she had little choice but to give this experimental therapy a try. “Sign me up,” she told Dr. Buck.
A Better Way to Target Cancer
Lutetium dotatate, now marketed under the name Lutathera, is one of several injectable radiation therapies now being tested or already in use. This form of precision medicine goes by a catchy name—theranostics—because it uses radioactive isotopes for both diagnostics and therapy. The special compounds are used to locate tumor cells and then to destroy them.
“Employing radioactive therapies against cancer isn’t new,” says Dr. Buck. “What has changed is the degree to which they can be precisely targeted to attack tumor cells while sparing healthy cells.”
Historically, Dr. Buck adds, the trouble has been that these treatments weren’t specific enough. “The hallmark of all of these therapies is that they emit very high energy radiation that extends over only a very short distance,” he says. “That’s perfect for going after cancer cells, but only if you can
direct them to exactly the right places, where the tumors are.”
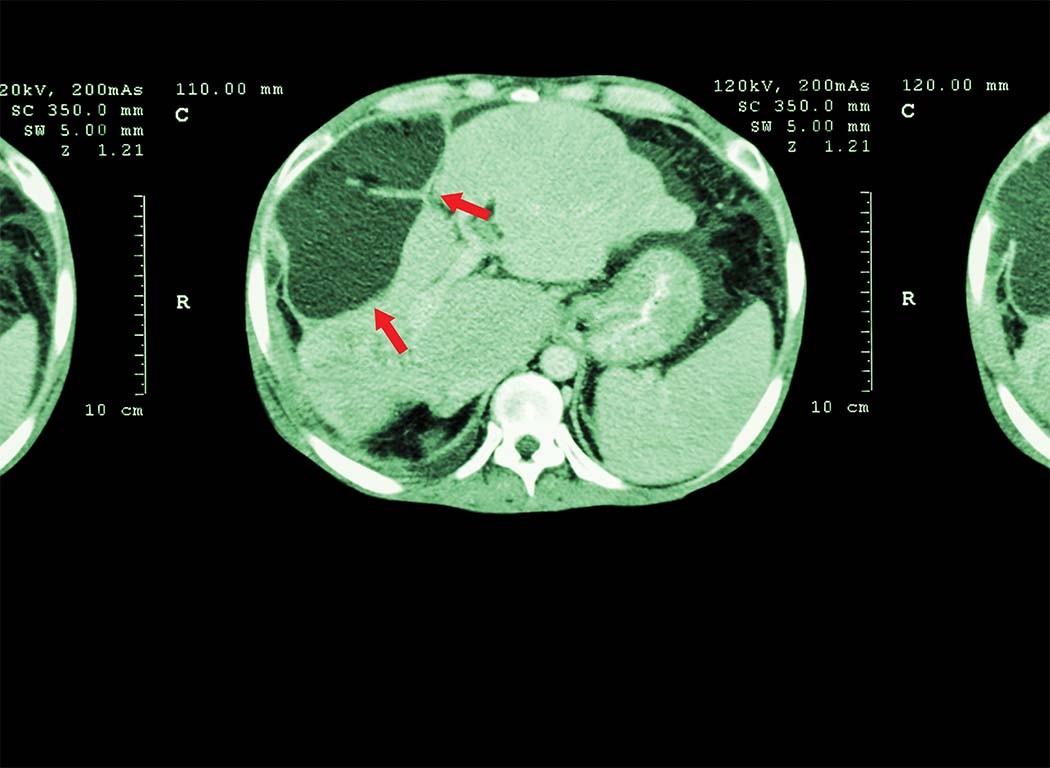
What you need to find, says Dr. Buck, is a kind of cellular receptor that exists only on tumor cells. The next challenge is to identify an imaging agent that can zero in on that particular receptor. In the case of carcinoid tumors, a kind of neuroendocrine tumor, that imaging agent is a radioactive compound known as gallium dotatate. After being injected, it seeks out and attaches itself to carcinoid tumor cells. Then, a positron emission tomography (PET) scan can show exactly where in the body the tumor cells are and how extensively the cancer may have spread.
That’s the diagnostic part, says Jackson Kiser, M.D., chief of molecular imaging in Carilion’s Department of Radiology. The big recent advances in nuclear medicine therapy came when researchers realized they could pair the precision of an imaging isotope such as gallium dotatate with other types of radioactive materials that can be used to destroy tumor cells, Dr. Kiser says.
That second kind of material includes alpha and beta emitters that can get into the machinery of cancer cells and disrupt their DNA, according to Dr. Kiser.
“Alpha emitters cause double-strand DNA breaks, destroying the DNA,” he says. “We don’t have many alpha-emitting therapeutics, but we have several kinds of beta emitters, which cause single-strand DNA breaks that destroy a cell’s DNA production. In both cases, they can render a tumor unable to replicate itself.”
To develop Lutathera, scientists removed the gallium in gallium dotatate and replaced it with lutetium, creating lutetium dotatate. “That pairing, of gallium dotatate and lutetium dotatate,” says Dr. Kiser, “was the breakthrough that made theranostics possible.”
Improvements in Quality of Life
Carcinoid tumors are rare, affecting only about 8,000 people a year in the United States, and they grow very slowly. That makes them a poor match for standard chemotherapy and radiation, which home in on cells that are dividing quickly. But carcinoid tumor cells do have a unique receptor, which can be targeted with a drug called octreotide. Even then, however, the effects tend to decrease over time.
In an important clinical trial, Lutathera was tested against an increased dose of octreotide to determine which did a better job of controlling patients’ carcinoid tumors. After two and a half years, octreotide was still working for only one in 10 patients. But the tumors of two-thirds of the patients who received Lutathera continued to be controlled after the same amount of time.
“It was a dramatically positive study,” says Dr. Buck. “And it got people excited about the possibilities for this kind of therapy.”
Now, although anyone with a carcinoid tumor will still be treated with octreotide initially, “the minute they progress, they now go on Lutathera,” says Dr. Buck.
Dr. Kiser notes that for many patients with these tumors, any relief is welcome. “Often, they’re just miserable,” he says. “Many have severe, almost constant diarrhea.” There’s a kind of preclinical trial called an expanded use protocol, also known as “compassionate use,” and when it was announced that Carilion, under that protocol, was going to be able to provide lutetium dotatate to a handful of patients, Dr. Kiser started hearing from people all over the country who were desperate to participate.
“I had to tell them we could only enroll six patients,” he says. “We had to see whether this thing would work.” But once Lutathera was approved, Carilion could treat anyone for whom it was an appropriate therapy. “We were among the first in the country to offer this,” says Dr. Kiser.
For most patients, Lutathera isn’t a cure, but it has extended patients’ lives and made them much more comfortable. “In the trials that were done in Europe, before this treatment came to the United States,” Dr. Kiser says, “patients were having up to five years of progression-free survival. That basically means that although the cancer is still there, you’ve rendered it unable to grow or spread. And for cancer, adding five years of progression-free survival is a home run.”
New Hope for Prostate Cancer
Now the search is on for other receptors that exist only on a particular kind of tumor cell, and not also on cells in healthy tissue. And one of the most exciting of those involves prostate cancer, the second-leading killer (after lung cancer) of men who die from cancer. In 2020, nearly 250,000 men in the United States were diagnosed with prostate cancer, and about 34,000 died from the disease.
The FDA recently approved two PET imaging drugs for men with prostate cancer that bind to something called prostate-specific membrane antigen, or PSMA. Because most prostate cancer cells seem to have elevated levels of the antigen, PSMA has emerged as an important target for prostate cancer imaging. That’s beneficial for diagnostic purposes, helping physicians see where a man’s cancer is and how far it has spread.
“Fortunately, we can approach this in the same way we go after neuroendocrine cancers,” says Dr. Kiser. “Once you’ve identified the extent of disease using a radiolabeled PSMA agent, you can take the diagnostic isotope off and put lutetium on.” That produces a therapeutic agent, lutetium-PSMA, that can seek out and destroy the cancer cells.
In June, results from a clinical trial of that compound in men who had exhausted other treatment options showed a six-month improvement in impeding the proliferation of cancer cells and a four-month improvement in survival.
“Those are significant gains in patients who had already failed hormone therapy and chemotherapy,” says Dr. Buck. But what if the theranostic agent were given earlier, in combination with—or even instead of—other therapies?
“Now they’re beginning to test when the best time is for this treatment,” says Dr. Buck. “Should we do it right after someone has failed hormone therapy? Should we do it when someone walks in the door with a prostate cancer diagnosis?”
Two large U.S. clinical trials are now examining the questions of when and how to use the PSMA theranostics approach.
What’s Next for Theranostics?
Dr. Kiser is extremely optimistic about what the future holds for theranostics. “This is simply one of the most exciting things to happen in cancer therapy,” he says. “The list of what can be treated is almost endless.”
Beyond neuroendocrine and carcinoid tumors and prostate cancer, that list includes lymphoma, meningioma, thyroid cancer, glioblastoma, and other malignancies.
“Breast cancer is one particularly promising frontier,” Dr. Kiser says, “as there can be three types of receptors, and some breast cancers have all three.” Those include receptors for estrogen and progesterone as well as for a growth factor called HER2.
There’s already an imaging agent that can help locate the estrogen receptor, and although it doesn’t yet have an associated therapeutic that could kill targeted tumor cells, Dr. Kiser and his team at Carilion have applied for intellectual property protection for such a compound that they hope to develop with a private company.
“What’s exciting is that you don’t have estrogen receptors just in breast cancer,” he says. “They’re also found in several other types of cancer. And you can target the progesterone receptor, and there’s a therapy, Herceptin, that targets the HER2 receptor. Think of the wallop you could pack with all of those therapies. You could really blow up the cancer.”
If a cancer has a specific receptor or a metabolic pathway associated with it, and if there’s an imaging agent that can target that receptor or pathway, “then you should be able to put something therapeutic, an alpha or beta emitter, on that agent,” Dr. Kiser says. “I call this designer therapy, because it’s specific to the patient. One patient with lung cancer might have one kind of receptor and another patient may have a different one. This way, you can give each of them the right therapy.”
Another fascinating possibility involves a diagnostic agent called fibroblast activation protein inhibitor, or FAPI. “Most kinds of cancer make a type 2 fibroblast; it’s something only cancers can produce,” says Dr. Kiser. “You can image the fibroblast with FAPI and basically see the extent of the disease. That gives you another way to image and potentially treat many kinds of cancer.”
There are potential risks involved with theranostics that need to be acknowledged or overcome, Dr. Kiser says. “Even when it’s targeted, radiation can cause collateral damage,” he says. “There can be bone marrow damage, particularly if you’re treating myeloma, which likes to live in the bone marrow.”
The radiation targeted to that tumor could harm the bone marrow, leading to a low count of white bloods cells or platelets. Radiation could also stay in the bloodstream and damage the kidneys as it makes its way into the urine and out of the body. But bone marrow tends to repair itself, and that’s why patients receive those infusions of amino acids, to protect the kidneys.
There’s also a problem of getting radioactive agents from the reactors or cyclotrons where they’re produced to the hospitals or clinics where they’re administered to patients. These are short-lived compounds, and time is of the essence in theranostics.
Yet there are few significant impediments to the kind of future for theranostics that Dr. Kiser and many others have described. And Carilion Clinic and Blue Ridge Cancer Care, pioneers in this approach to treating cancer, expect to be at the center of those advances. Additional research collaborations offer the opportunity for other radiotracers and radiotherapeutics to be developed in the Roanoke region, and Carilion is building new infusion centers and reaching out to global partners.
“We want to be one of the superior sites in the country for these therapies,” Dr. Kiser says.
Enjoying Life with the Grandkids

Anita Haymaker’s treatment with Lutathera has exceeded almost everyone’s expectations. “I can’t say that I’m cured,” she says. But four years after she first spoke with Dr. Buck, her cancer is almost completely gone, and so far, her periodic scans have shown no progression.
Haymaker, now 76, spent part of this past summer with her grandchildren. “We live at the lake,” she says, “and they go in and out of the water the entire time.”
By David Bumke
