Supporting Our System
Our Applied Human Factors team works within the Carilion system to examine how workload, capacity, and environmental design interact to shape clinical performance, safety, and experience.
By studying how work is actually carried out—across varying levels of demand, staffing, and ph...
Workload
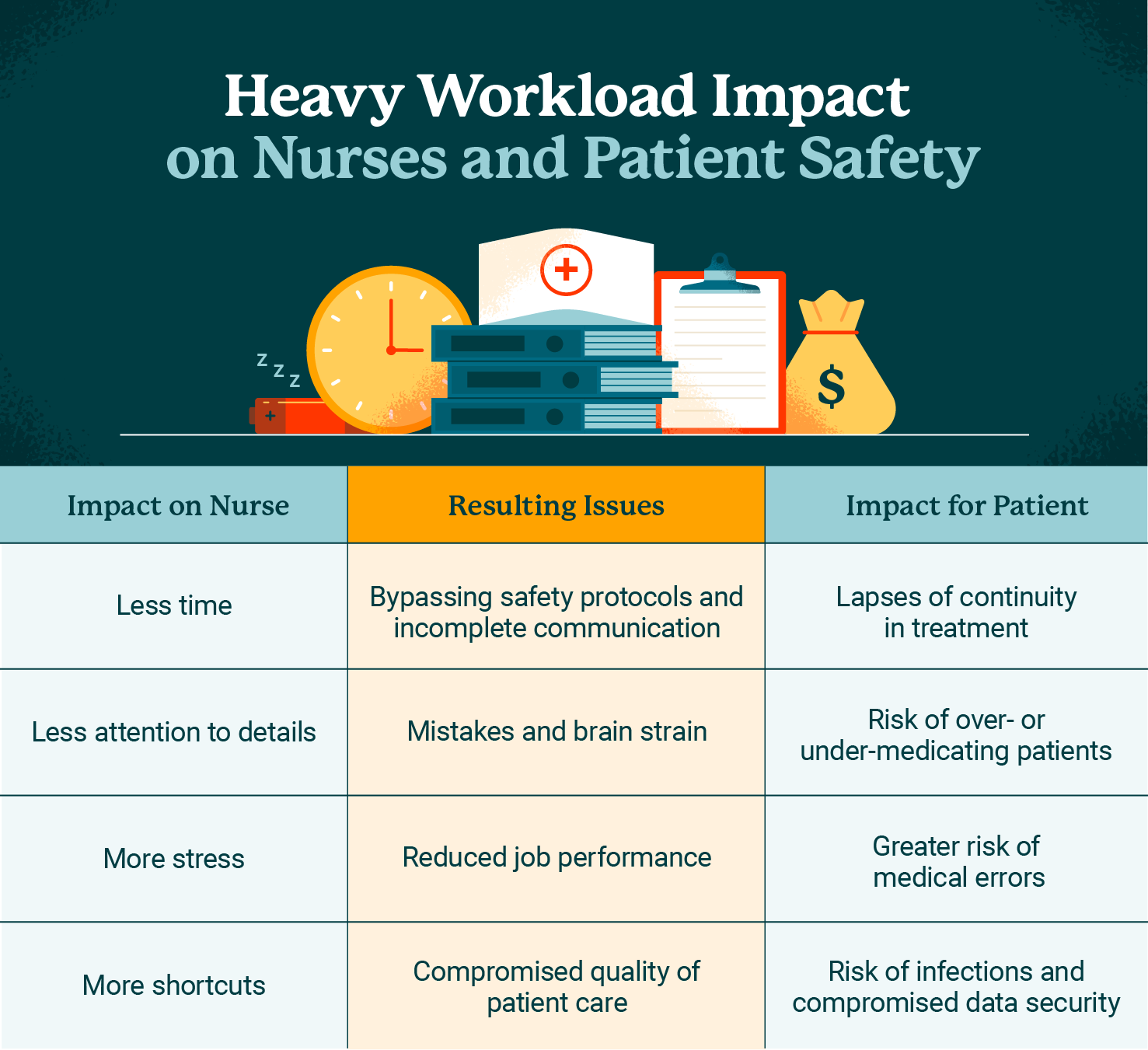
Our Applied Human Factors department focuses on understanding how work is actually done in complex clinical environments and how variations in workload affect performance, safety, and outcomes. By examining factors such as task density, interruptions, cognitive load, staffing patterns, and system design, our team seeks to identify when routine variability turns into excessive workload that exceeds human capacity.
When workload outpaces capacity, clinicians are forced to adapt—often through workarounds, care rationing, or reliance on memory under pressure—which increases the risk of error, delays, and missed care. Applied human factors brings a scientific, systems-based lens to these challenges, moving beyond individual blame to uncover how design, processes, and organizational decisions shape frontline performance.
This work directly supports quality improvement by identifying high-risk conditions before harm occurs and by informing the design of safer, more resilient workflows, tools, and environments. By aligning systems with human capabilities and limitations, our team aims to reduce preventable harm while improving efficiency and reliability of care delivery. At the same time, addressing workload-capacity mismatches supports both patient and provider satisfaction: patients experience more consistent, attentive care, and clinicians benefit from reduced burnout, clearer priorities, and a greater sense of control and professional fulfillment. In this way, applied human factors serves as a critical bridge between operational improvement, patient safety, and the well-being of the healthcare workforce.
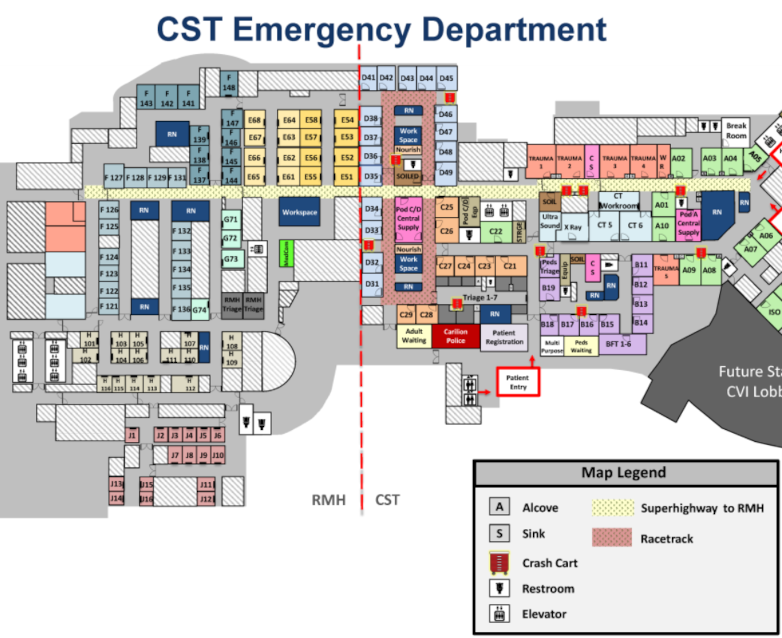
Enivronmental Design
Environmental design plays a critical role in shaping clinical workflow and influencing both physical and cognitive workload. The layout of care spaces, visibility of patients and equipment, proximity of supplies, lighting, noise levels, and ergonomics all affect how efficiently and safely work can be performed.
Poorly designed environments increase unnecessary movement, interruptions, and information gaps, forcing clinicians to spend time and mental energy navigating the space rather than focusing on patient care. Over time, these design-related inefficiencies compound workload, contributing to fatigue, delays, and increased risk of error—especially in high-acuity or fast-paced settings.
Our team evaluates our different care environments as active components of the work system, not a neutral backdrop. By studying how clinicians interact with physical spaces in real-world conditions, we aim to identify design features that support performance or redesign those that hinder it.
Evidence-informed improvements—such as optimizing room layouts, standardizing supply locations, improving line-of-sight, and reducing noise and clutter—can streamline workflows and reduce cognitive burden. These changes enhance quality and safety while also improving provider satisfaction by making work less frustrating and more intuitive, ultimately enabling teams to deliver better care with less strain.